Stomach Inflammatory Fibroid Polyp (IFP)
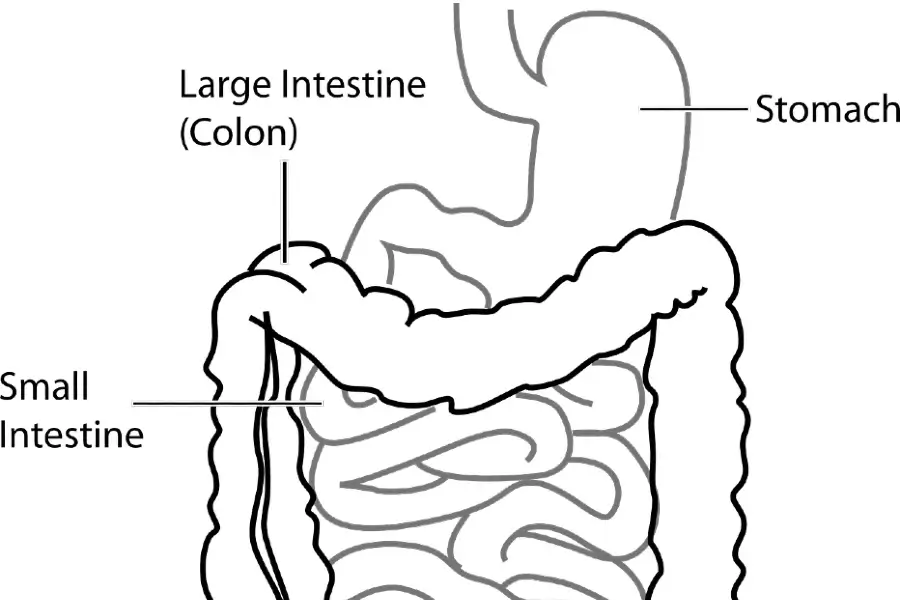
An inflammatory fibroid polyp (IFP) is an uncommon, benign (noncancerous) tumor that can form in the stomach wall. It is most usually found in the stomach lining (gastric mucosa). However, it can also appear in the esophagus, small intestine, large intestine, and gallbladder.
Here’s what you should know about stomach IFP:
Symptoms:
IFPs of the stomach rarely cause symptoms and are typically discovered inadvertently during an endoscopy performed for another reason. However, if the polyp becomes large enough, it may produce some of the following symptoms:
- Abdominal Pain
- Nausea
- Vomiting
- Bleeding (rare)
- Feeling of a lump in the belly (rare)
- Blockage of the stomach exit (rare) in extreme situations
Diagnosis:
Doctors often diagnose IFPs using a combination of:
Endoscopy: An endoscopic check, such as an upper endoscopy or gastroscopy, allows the doctor to see into the stomach and possibly collect a biopsy (tissue sample) for further analysis under a microscope.
Biopsy: A microscopic analysis of the biopsied tissue is required to confirm the diagnosis and distinguish IFP from other types of cancers.
Treatment: The suggested treatment for stomach IFPs is determined by the size and location of the polyp, as well as the presence or absence of symptoms.
Endoscopic removal is frequently preferred for smaller polyps due to its minimum invasive nature and potential for better patient results. A gastroenterologist or another qualified healthcare expert normally carries out this operation. During endoscopic polyp removal, the healthcare professional inserts a thin, flexible tube called an endoscope into the patient’s mouth or nose. The endoscope contains a small camera at the tip that allows the provider to see the polyp and the surrounding parts of the digestive tract. Once the polyp has been identified, the healthcare provider will utilize specialized tools and instruments passed via the endoscope to grasp, capture, and remove it.
Endoscopic polyp removal is usually regarded as a safe and successful method for removing tiny polyps.
These implements may include small forceps, snares, or other cutting devices created specifically for this purpose. To ensure the patient’s comfort and minimize discomfort, the entire treatment is performed while they are sedated or under local anesthesia.
The resected polyp is then sent to a laboratory for additional examination to assess its characteristics and detect any potential underlying diseases or risks. This information can assist the healthcare professional in designing an appropriate treatment plan and continuing to monitor the patient’s condition.
Endoscopic polyp removal is usually regarded as a safe and successful method for removing tiny polyps. It eliminates the need for more intrusive surgical procedures and helps the patient recuperate faster.
However, the healthcare provider will carefully consider the size, location, and other criteria to determine whether this method is best for each patient.
Surgery:
In some circumstances, surgery may be required to remove the polyp, especially for larger polyps or those that cause difficulties. The unique situation will determine the sort of surgery required.
Prognosis:
IFPs are benign tumors, and the prognosis following total removal is often favorable. Regular follow-up endoscopies may be recommended to check for recurrence. If you are concerned about a stomach IFP, visit a healthcare expert for diagnosis and treatment.