Evidence-Based Insights: How to Differentiate Between IBS and IBD for Better Patient Outcomes
Overview of Digestive Disorders
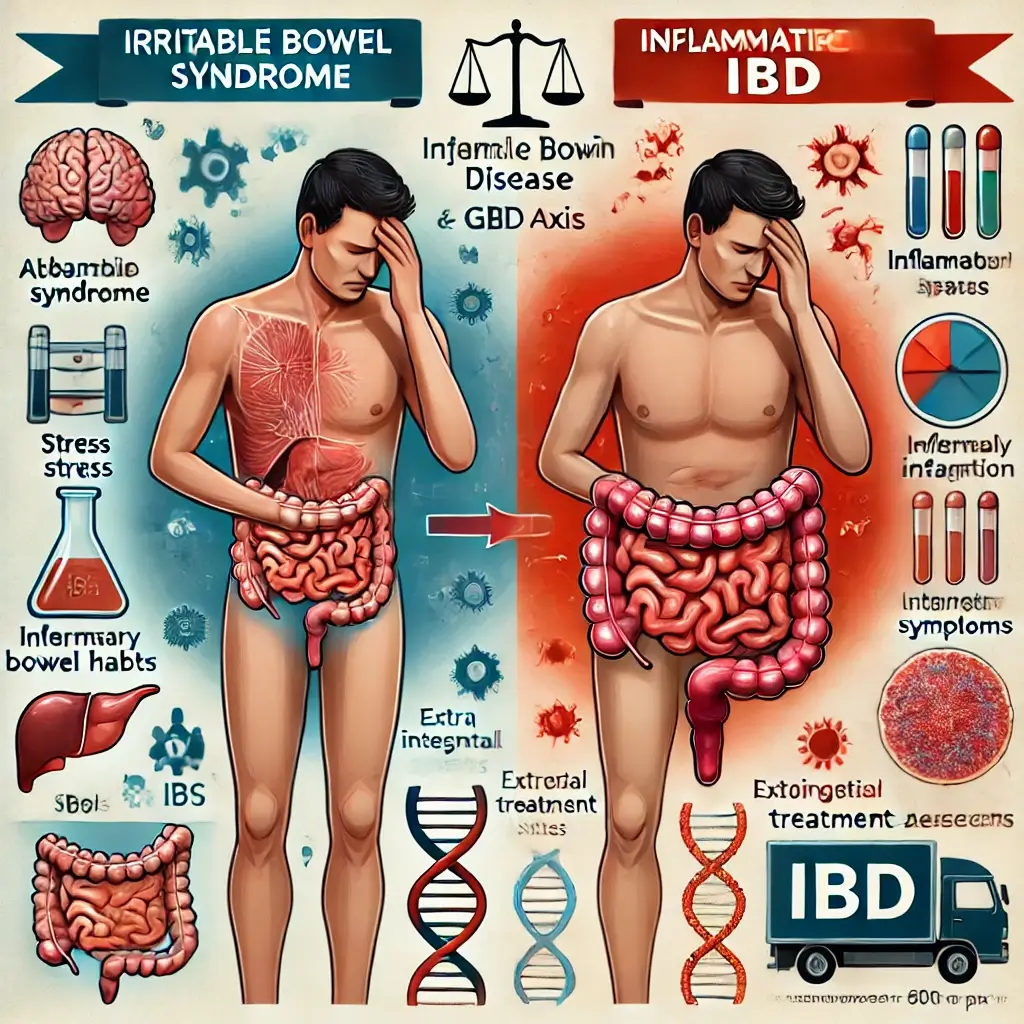
Digestive disorders healthcare systems pose significant challenges to healthcare systems worldwide, with millions of people experiencing symptoms like abdominal pain and altered bowel habits, and bloating. Among the most commonly discussed conditions are Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD). Despite their similarities in symptom presentation and clinical management, these disorders differ markedly in etiology, pathology, and management. Recognizing these distinctions is crucial for clinicians, patients, and researchers.
Functional vs. Autoimmune Conditions
IBS is categorized as a functional gastrointestinal disorder, meaning its symptoms result from abnormal functioning rather than structural damage. IBD, on the other hand, is a chronic autoimmune condition characterized by inflammation and physical damage to the digestive tract. The distinction is not just academic—it directly informs diagnostic approaches and treatment strategies, and long-term patient outcomes.
Purpose and Scope
This article provides a clinical comparison of IBS and IBD, supported by recent medical research and evidence-based treatment approaches. Understanding these conditions from a clinical and research-focused perspective can aid healthcare professionals and patients in making informed decisions.
Clinical and Pathological Distinctions
1. Pathophysiology
IBS Pathophysiology
IBS is linked to disruptions in the gut-brain axis, abnormal intestinal motility, and visceral hypersensitivity. Studies have shown that IBS may also involve dysbiosis and gut microbiota imbalance, as well as low-grade inflammation in some patients. Psychological factors such as anxiety and depression in gastrointestinal health often exacerbate symptoms, highlighting the interplay between mental and gastrointestinal health.
IBD Pathophysiology
IBD involves an immune-mediated inflammatory response, with Crohn’s disease and ulcerative colitis being the primary subtypes. The immune system attacks the gastrointestinal lining, leading to chronic inflammation and structural damage. Genetic predisposition and environmental factors, such as diet and pathogen exposure in IBD development, play significant roles in its development.
Symptom Profiles Overview
2. Symptom Profiles
IBS Symptoms in Detail
Patients with IBS typically report abdominal pain and irregular bowel habits (diarrhea, constipation, or alternating). These symptoms often improve after a bowel movement and are exacerbated by stress and dietary triggers. Notably, IBS does not cause rectal bleeding, fever, or significant weight loss.
IBD Symptoms in Detail
IBD presents with severe and persistent gastrointestinal symptoms, including chronic diarrhea, rectal bleeding, abdominal pain, fatigue, and unintentional weight loss. Patients may also experience extraintestinal manifestations and complications such as joint pain, skin rashes, and eye inflammation. Complications like strictures and increased colorectal cancer risk distinguish IBD from IBS.
Diagnostic Approaches
3. Diagnostic Tools
IBS Diagnostic Methods
Diagnosing IBS relies on symptom-based criteria and Rome IV guidelines, and the exclusion of other conditions through stool tests, blood work, and imaging. Psychological assessments in IBS diagnosis may also be included to address associated mental health factors.
IBD Diagnostic Methods
IBD diagnosis requires invasive procedures and imaging studies like colonoscopy with biopsies and imaging studies. Laboratory tests, including C-reactive protein and fecal calprotectin measurements, help identify inflammation and disease activity. Genetic testing and biomarker development are emerging tools in IBD diagnosis and prognosis.
Treatment Approaches
Treatment Strategies
IBS Treatment Strategies
1. IBS Management IBS treatment focuses on symptom control and quality of life improvement. Key approaches include:
Dietary Adjustments: The low-FODMAP diet for symptom reduction has shown efficacy in reducing symptoms by limiting fermentable carbohydrates.
Medications: Antispasmodics and visceral hypersensitivity medications are commonly used.
Psychological Interventions: Cognitive-behavioral therapy and gut-directed hypnotherapy have been effective in addressing the gut-brain axis.
IBD Treatment Strategies
2. IBD Management The primary goals of IBD treatment are to reduce inflammation and achieve remission. Approaches include:
Pharmacologic Therapies: Anti-inflammatory drugs and immune modulators are mainstays of treatment.
Dietary Interventions: Exclusive enteral nutrition and elimination diets may support remission in specific cases.
Surgical Interventions: For patients with severe disease or complications, surgeries like colectomy for severe IBD may be necessary.
Research Developments
Recent advancements are reshaping the management of both IBS and IBD:
Microbiome Research: Studies on gut microbiota and fecal microbiota transplantation have led to innovations which show promise for both conditions.
Personalized Medicine: Genetic profiling and biomarker development in IBD treatment are enabling tailored treatments for IBD patients.
Psychosocial Interventions: Integrating mental health care in IBS management has demonstrated significant improvements in symptom management.
Final Insights
IBS and IBD represent two distinct yet impactful gastrointestinal disorders, each requiring unique diagnostic and treatment approaches. While IBS is a functional disorder with gut-brain disruptions, IBD is an autoimmune condition with systemic implications. Advances in research, from microbiome studies to personalized medicine applications, are providing new avenues for managing these conditions effectively.
Recommendations
For patients and healthcare providers, understanding the nuanced differences between IBS and IBD is essential for achieving better health outcomes. If you experience persistent digestive symptoms, consult a healthcare provider to determine the underlying cause and develop a targeted treatment plan.
References
[References section remains unchanged]